Introduction.
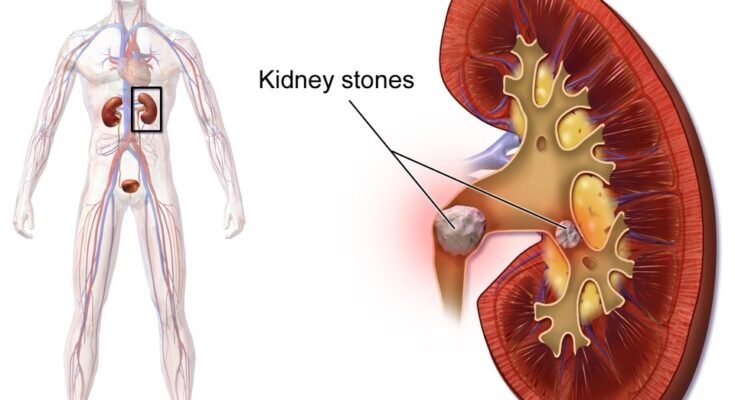
A kidney stone is a hard deposit made of minerals and salts that form inside the kidneys. This condition is called nephrolithiasis or urolithiasis.
Kidney stones have a wide range of sizes, and some may form without being noticed. Small kidney stones are often viable, and larger stones may block urine flow and cause pain. Kidney stones occur across the lifespan of a person, but are primarily seen in adults, especially men. The majority of kidney stones can be prevented or treated with lifestyle changes, diet, and modern medicine
- A condition where hard deposits form inside the kidney.
- Also called renal calculi or nephrolithiasis.
- Made of salt and minerals.

Photo by Jakupica via Wikimedia Commons, CC BY-SA 4.0
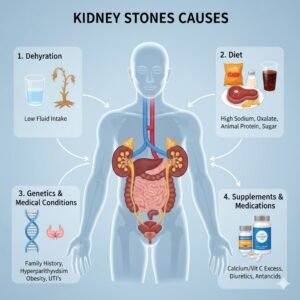
Causes.
Kidney stones form when urine becomes concentrated, allowing minerals to crystallize and stick together. Risk factors include:
- Dehydration leading to concentrated urine.
- High intake of salt, protein, or sugar.
- Family history of kidney stones.
- Certain medical conditions, like gout.
- Medications (diuretics, calcium-based antacids, etc.).
- Obesity
Types of Kidney Stones.
-
Calcium stones
Calcium stones represent the most prevalent variety of kidney stone, accounting for approximately 70-80 percent of all cases. They typically form when calcium is excreted excessively from the blood, with a crystallizing agent such as oxalate or phosphate. A substance is often overrepresented in the urine, and when a threshold is met, that flavour of mineral will precipitate as a crystallized stone in the kidneys. An excess calcium dietary intake or medical disorders can lead to urinary calculus formation. Factors such as dehydration, excessive dietary oxalate ingestion (spinach, nuts, chocolate), excessive sodium intake, some metabolic disorders (e.g., hyperparathyroidism), and a family history of urinary calculi can increase the likelihood of urinary calcium deposition as stones. If a stone gets large enough, it can lead to extreme pain, blood in the urine (hematuria), and obstructive features. The typical treatment for a non-obstructive stone is habitual attempts to drink frequent amounts of water to remove any deposits – the urinary stones are so small they usually can pass within 3-4 hours. If they have an impaired urine flow, it often requires shock wave lithotripsy or surgical removal. Using preventive measures is, in fact, quite easy – remain hydrated with good fluid intake, avoid things like sodium and oxalate-rich foods, and potentially employ medications that stabilize excretion of calcium from urine.
-
Uric acid stones
Uric acid stones develop when the acidity of urine causes uric acid to precipitate out of solution. They are associated with gout, obesity, dehydration, and diets high in protein. These stones can produce sharp pain in the back or side, blood in the urine, and frequent urination. Uric acid stones usually do not show on X-ray, though CT or ultrasound will identify them; calcium stones will show on X-ray. Treatment consists of drinking water and using medications to alkalize urine; potassium citrate would be an example. Allopurinol may be prescribed to lower uric acid levels. Uric acid prevention is associated with hydration, frequency of food intake, and avoiding foods with high purine levels.
-
Struvite stones
These stones can grow very quickly, and they can grow very large, even filling the kidney. They can present with back pain, fever, difficulty urinating, and cloudy urine. They are more common in women than men because of the increased occurrence of UTIs overall. Struvite stones can be treated with lithotripsy when required, but rarely pass on their own, so removal tends to be surgical. Prevention tends to be based on accurately treating UTIs and possibly administering prophylactic antibiotics.
-
Cystine stones
Cystine stones are infrequent kidney stones resulting from an inherited condition known as cystinuria.
This ailment causes the kidneys to leak too much cystine (an amino acid) in the urine.
When there is too much cystine, excess cystine will gather together to form crystals that form hard stones.
Cystine stones typically occur in childhood or early adult years and appear to recur multiple times.
Symptoms include flank pain that is most severe, hematuria (blood in the urine), and urinary obstruction.
Treatment components include drinking lots of water and drugs that help to reduce the amount of cystine found in the urine.
Lifestyle is focused on taking in large amounts of fluids on a daily basis and on taking special medication to dissolve (and/or avoid) stones.

Symptoms.
Many affected individuals will present to Urgent Care or the emergency room with associated signs indicating kidney stones—like hematuria—which may appear as pink, red, brown urine, pain or burning with urination, frequent feelings of urgency to urinate, and, in many cases, cloudy, foul-smelling urine. The patient may also present with accompanying feelings of nausea, vomiting, or difficulty passing urine, especially if there is a blockage. If the process becomes complicated by an infection, the patient may present even more severely symptomatic with fevers and chills, and should be treated urgently. Here are some major symptoms:
- Severe pain in the side/back (flank pain), radiating to the lower abdomen or groin.
- Pain radiating to the lower abdomen and groin.
- Pain during urination.
- Blood in urine.
- Frequent urination and nausea.
- Cloudy or foul-smelling urine.
Diagnosis.
A patient needing to find out if they have kidney stones will usually go through a typical process for the diagnosis of kidney stones. The medical professional will take an initial history, and then do a physical examination, followed by a workup, and finally a follow-up. Routine workups include urinalysis, which looks for blood, crystals, or evidence of infection in the urine, and blood tests to check for high calcium or uric acid levels or other contributing substances. Imaging studies are the best way to confirm kidney stones. An ultrasound is usually the first choice, but CT scans are much more detailed in showing the size, number of stones, and location of stone(s). Traditionally, there were also KUB and IVP, but these imaging studies are not as commonly utilized now. Obtaining a thorough and accurate diagnosis is critical not only to determine the presence of stones but to suggest the best treatment.
- Urine test to check for crystals.
- Blood test for calcium and uric acid.
- CT scan or ultrasound imaging.
- Analysing of passed stones.
Treatment.
The treatment depends on the size of the kidney stones. For larger or more painful stones, procedures may need to be completed. ESWL is a procedure to break stones up into smaller pieces by using sound waves and place the pieces into a state of passage. Another medical procedure is ureteroscopy. In ureteroscopy, a very thin scope is passed through the urethra and bladder to the ureter to either remove or reduce the stone. In extreme cases, another treatment, called percutaneous nephrolithotomy, is performed, which is the minimally invasive surgical removal of a large kidney stone from within the kidney. Also, sometimes for the prevention of a specific type of stone, medications such as allopurinol or potassium citrate can be prescribed for the patient. Along with treatment, usually dietary habits and hydration are suggested to the individual as a measure of prevention
- Drinking plenty of water to flush out stones.
- Pain relievers and medications.
- Shock wave lithotripsy (breaking stones).
- Surgery in severe cases.
- Ureteroscopy: the scope removes or breaks the stone.
- Percutaneous nephrolithotomy: surgery for very large stones.
- Medications: for uric acid or cystine stones (e.g., allopurinol, potassium citrate).
Prevention.
- Stay hydrated by drinking enough water.
- Limit salt, sugar, and animal protein intake.
- Eat calcium-rich foods moderately.
- Maintain a healthy body weight.
- Drink 8–12 glasses of water daily.
- Eat more fruits and vegetables.
- Follow the doctor’s advice if prone to recurring stones.
Conclusion.
- Kidney stones are preventable with lifestyle changes.
- Early diagnosis helps reduce complications.
- Proper hydration is the key to prevention.